Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein. This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER. Primary lung tumors are rare in children and histologically quite diverse.[1] A review of primary malignant epithelial lung tumors using the National Cancer Database found that the most common primary malignant pediatric lung neoplasms were carcinoid tumors (63%), followed by mucoepidermoid carcinoma of the lung (18%).[2] Tracheobronchial tumors are a heterogeneous group of primary endobronchial lesions. Although adenoma implies a benign process, all varieties of tracheobronchial tumors occasionally display malignant behavior. Most primary lung tumors are malignant. In a review of 383 primary pulmonary neoplasms in children, 76% were malignant and 24% were benign.[3] The following histological types have been identified (see Figure 1):[4,5,6,7,8,9,10] References: When epithelial cancers of the lung occur, they tend to be of advanced stage. Prognosis is dependent on both histology and stage.[1] The presenting symptoms of tracheobronchial tumors are usually caused by an incomplete tracheobronchial obstruction and include the following: Because of difficulties in diagnosis, symptoms are frequently present for months. Occasionally, children with wheezing are treated for asthma, and diagnosis can be delayed for as long as 4 to 5 years.[2] Metastatic lesions are reported in approximately 6% of patients with carcinoid tumors, and recurrences are reported in 2% of cases. Atypical carcinoid tumors are rare but more aggressive, and 50% of these patients present with metastatic disease at diagnosis.[1,3] One study reported a single child with a carcinoid tumor and metastatic disease who developed the classic carcinoid syndrome.[4] Octreotide nuclear scans may demonstrate uptake of radioactivity by the tumor or lymph nodes, suggesting metastatic spread. References: The management of tracheobronchial tumors is somewhat controversial because tracheobronchial tumors are usually visible endoscopically. Biopsy of these lesions may be hazardous because of the risk of hemorrhage. New endoscopic techniques have allowed biopsy to be performed more safely.[1,2] However, endoscopic resection is not recommended except in highly selected cases.[2,3,4] Bronchography or computed tomography may be helpful to determine the degree of bronchiectasis distal to the obstruction since the degree of pulmonary destruction may influence surgical therapy.[5] References: With the exception of rhabdomyosarcomas, tracheobronchial tumors of all histological types are associated with an excellent prognosis after surgical resection in children, even in the presence of local invasion.[1,2]; [3][Level of evidence B4] References: The treatment of choice is conservative pulmonary resection, including sleeve segmental resection (when feasible), with the removal of the involved lymphatics.[1,2]; [3][Level of evidence B4] Chemotherapy and radiation therapy are not indicated for tracheobronchial tumors, unless evidence of metastasis is documented or the tumor is a rhabdomyosarcoma. Treatment options for tracheobronchial tumors, according to histological type, are as follows: Carcinoid Tumors (Neuroendocrine Tumors of the Bronchus) The treatment of choice is surgical resection with lymph node sampling. The overall survival rate is higher than 90% for these patients.[4,5,6] One study reported no deaths among patients who did not have lymph node involvement, and the 10-year survival rate was 89% for patients with one or more involved lymph nodes.[6] Mucoepidermoid Carcinomas The recommended treatment is open surgical resection and lymph node sampling. Endoscopic resection is not recommended.[7,8] Inflammatory Myofibroblastic Tumors The treatment of choice is surgery. However, if the tumor has an ALK variant, treatment with crizotinib may be effective.[8,9,10,11] Rhabdomyosarcomas Surgery is not indicated. These tumors are very responsive to chemotherapy and radiation therapy, even with lymph node metastasis.[8] For more information, see Childhood Rhabdomyosarcoma Treatment. Granular Cell Tumors Surgical resection is based on morbidity risk.[8,12,13] For information about other neuroendocrine carcinoid tumors, see Pediatric Gastrointestinal Neuroendocrine Tumors Treatment. References: Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, see the ClinicalTrials.gov website. Cancer in children and adolescents is rare, although the overall incidence has slowly increased since 1975.[1] Children and adolescents with cancer should be referred to medical centers that have a multidisciplinary team of cancer specialists with experience treating the cancers that occur during childhood and adolescence. This multidisciplinary team approach incorporates the skills of the following pediatric specialists and others to ensure that children receive treatment, supportive care, and rehabilitation to achieve optimal survival and quality of life: For specific information about supportive care for children and adolescents with cancer, see the summaries on Supportive and Palliative Care. The American Academy of Pediatrics has outlined guidelines for pediatric cancer centers and their role in the treatment of children and adolescents with cancer.[2] At these centers, clinical trials are available for most types of cancer that occur in children and adolescents, and the opportunity to participate is offered to most patients and their families. Clinical trials for children and adolescents diagnosed with cancer are generally designed to compare potentially better therapy with current standard therapy. Other types of clinical trials test novel therapies when there is no standard therapy for a cancer diagnosis. Most of the progress in identifying curative therapies for childhood cancers has been achieved through clinical trials. Information about ongoing clinical trials is available from the NCI website. Dramatic improvements in survival have been achieved for children and adolescents with cancer. Between 1975 and 2020, childhood cancer mortality decreased by more than 50%.[3,4,5] Childhood and adolescent cancer survivors require close monitoring because side effects of cancer therapy may persist or develop months or years after treatment. For information about the incidence, type, and monitoring of late effects in childhood and adolescent cancer survivors, see Late Effects of Treatment for Childhood Cancer. Childhood cancer is a rare disease, with about 15,000 cases diagnosed annually in the United States in individuals younger than 20 years.[6] The U.S. Rare Diseases Act of 2002 defines a rare disease as one that affects populations smaller than 200,000 people in the United States. Therefore, all pediatric cancers are considered rare. The designation of a rare tumor is not uniform among pediatric and adult groups. In adults, rare cancers are defined as those with an annual incidence of fewer than six cases per 100,000 people. They account for up to 24% of all cancers diagnosed in the European Union and about 20% of all cancers diagnosed in the United States.[7,8] In children and adolescents, the designation of a rare tumor is not uniform among international groups, as follows: Most cancers in subgroup XI are either melanomas or thyroid cancers, with other cancer types accounting for only 2% of the cancers diagnosed in children aged 0 to 14 years and 9.3% of the cancers diagnosed in adolescents aged 15 to 19 years. These rare cancers are extremely challenging to study because of the relatively few patients with any individual diagnosis, the predominance of rare cancers in the adolescent population, and the small number of clinical trials for adolescents with rare cancers. References: The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above. Editorial changes were made to this summary. This summary is written and maintained by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® Cancer Information for Health Professionals pages. Purpose of This Summary This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the treatment of childhood tracheobronchial tumors. It is intended as a resource to inform and assist clinicians in the care of their patients. It does not provide formal guidelines or recommendations for making health care decisions. Reviewers and Updates This summary is reviewed regularly and updated as necessary by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH). Board members review recently published articles each month to determine whether an article should: Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary. The lead reviewers for Childhood Tracheobronchial Tumors Treatment are: Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website's Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries. Levels of Evidence Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Pediatric Treatment Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations. Permission to Use This Summary PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary]." The preferred citation for this PDQ summary is: PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Tracheobronchial Tumors Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/lung/hp/child-tracheobronchial-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 31593395] Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images. Disclaimer Based on the strength of the available evidence, treatment options may be described as either "standard" or "under clinical evaluation." These classifications should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page. Contact Us More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's Email Us. Last Revised: 2025-01-06 This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Ignite Healthwise, LLC.Topic Contents
Childhood Tracheobronchial Tumors Treatment (PDQ®): Treatment - Health Professional Information [NCI]
Types of Childhood Tracheobronchial Tumors
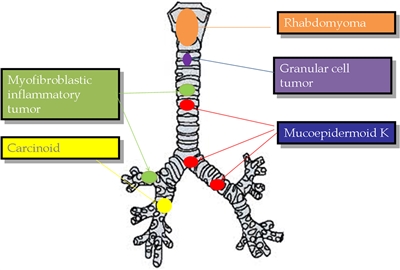
Figure 1. The most representative primary tracheobronchial tumors are described with their more frequent location. Reprinted from Seminars in Pediatric Surgery, Volume 25, Issue 3, Patricio Varela, Luca Pio, Michele Torre, Primary tracheobronchial tumors in children, Pages 150–155, Copyright (2016), with permission from Elsevier.Clinical Presentation
Diagnostic Evaluation
Prognosis
Treatment of Childhood Tracheobronchial Tumors
Treatment Options Under Clinical Evaluation for Childhood Tracheobronchial Tumors
Special Considerations for the Treatment of Children With Cancer
Latest Updates to This Summary (01 / 06 / 2025)
About This PDQ Summary
Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.Childhood Tracheobronchial Tumors Treatment (PDQ®): Treatment - Health Professional Information [NCI]



