Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein. This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER. Hereditary leiomyomatosis and renal cell cancer (HLRCC) is characterized by the presence of one or more of the following: cutaneous leiomyomas (or leiomyomata), uterine leiomyomas (fibroids) in females, and renal cell cancer (RCC). Germline pathogenic variants in the FHgene are responsible for the susceptibility to HLRCC. FH encodes fumarate hydratase, the enzyme that catalyzes the conversion of fumarate to malate in the tricarboxylic acid cycle (Krebs cycle). Nomenclature Historically, the predisposition to the development of cutaneous leiomyomas was referred to as multiple cutaneous leiomyomatosis. In 1973, two kindreds were described in which multiple members over three generations exhibited cutaneous leiomyomas and uterine leiomyomas and/or leiomyosarcomas inherited in an autosomal dominant pattern.[1] That report also described a woman aged 20 years with uterine leiomyosarcoma and metastatic RCC. Subsequently, the association of cutaneous and uterine leiomyomas became known as Reed syndrome. However, the clear association of cutaneous leiomyomas and RCC was not described until 2001, when a study reported two Finnish families in whom cutaneous and uterine leiomyomas and papillary type 2 RCC cosegregated [2] and the name hereditary leiomyomatosis and renal cell cancer (HLRCC) was introduced. References: FHGene The FHgene consists of ten exons encompassing 22.15 kb of DNA. The gene is highly conserved across species. The human FH gene is located on chromosome 1q42.3-43. Hereditary leiomyomatosis and renal cell cancer (HLRCC) is an autosomal dominant syndrome. An individual can be predisposed to HLRCC disease manifestations when he/she inherits a heterozygous pathogenic variant in the FH gene.[1] Various FH pathogenic variants have been identified in families with HLRCC. Most are missense variants. However, nonsense variants, frameshift variants, splice-site variants, and whole-gene/partial deletions have also been identified and described.[2,3,4,5,6] Renal tumors that develop in individuals who inherit a germline pathogenic variant in FH typically display a loss of heterozygosity because of a second somatic FH variant. This finding suggests that loss of function of the fumarate hydratase protein is the basis for tumor formation in HLRCC and supports a tumor suppressor function for FH.[2,7] Inherited biallelic pathogenic variants in the FH gene (homozygous or compound heterozygous) can cause autosomal recessive fumarate hydratase deficiency (FHD) (also abbreviated as FMRD), a disorder characterized by rapid, progressive neonatal neurological impairment that includes hypotonia, seizures, and cerebral atrophy. For more information, see the Genetically Related Disorders section. Prevalence Prevalence estimates for HLRCC are evolving. Older estimates suggested a prevalence of 1 in 200,000 individuals.[8] However, an analysis of nonpopulation-based cohorts found an FHcarrier frequency of 1 in 1,000 individuals, suggesting a larger number of asymptomatic cases than previously thought.[9] A clinical database analysis of over 120,000 records from individuals undergoing hereditary cancer genetic testing estimated a carrier frequency of 1 in 2,668 (0.04%). These estimates reflect the high rate of FH pathogenic variants that were detected incidentally in individuals undergoing cancer genetic testing for other indications. This finding suggests that HLRCC may be one of the most common hereditary cancer syndromes.[10] Penetrance ofFHPathogenic Variants On the basis of the observation that most patients with HLRCC have at least one of the three major clinical manifestations, the penetrance of HLRCC in carriers of pathogenic FH variants appears to be very high. However, the estimated cumulative lifetime incidence of renal cell cancer (RCC) varies widely, with most estimates ranging from 15% to 30% in families with germline FH pathogenic variants, depending on ascertainment method and the imaging modalities used.[3,4,7,11,12,13] A 2020 study showed that FH pathogenic variants have been detected at a higher rate than previously thought, indicating that lifetime risk of kidney cancer in individuals with HLRCC may be significantly lower than current estimates suggest.[9] A study that analyzed patients undergoing cancer genetic testing suggested that RCC may be more common in males with HLRCC than in females with HLRCC.[10] Several studies have also reported an enrichment of FH germline pathogenic variants in individuals with RCC and African ancestry.[10,14] Genotype-Phenotype Correlations Correlations between specific FH variants and the occurrence of cutaneous/uterine leiomyomas, RCC, or other primary features of HLRCC have not been reported.[4] However, certain FH variants (primarily missense variants) seem to be associated with an increased risk for paraganglioma (PGL)/pheochromocytoma (PHEO) in the absence of other HLRCC features.[15] Three recurrent variants with increased PGL/PHEO risk have been reported in the literature: (1) p.Thr234Ala, (2) p.Ala273Thr, and (3) p.Ala194Thr. Conversely, FH variants associated with autosomal dominant HLRCC and autosomal recessive FHD do not seem to correlate with increased PGL/PHEO risk. Although PGL/PHEO surveillance is not included in HLRCC guidelines, the authors suggest that surveillance similar to that which is recommended for SDHx carriers may be warranted. For more information, see the Surveillance section. Sequence Analysis Using bidirectional DNA sequencing methodology, pathogenic variants in FH have been detected in more than 85% of individuals with HLRCC.[3,4,16] Genetically Related Disorders Fumarate hydratase deficiency (fumaric aciduria, FHD) FHD (also abbreviated as FMRD) is an autosomal recessive disorder that results from the inheritance of biallelic pathogenic variants in the FH gene. This inborn error of metabolism is characterized by rapid, progressive neurological impairment that includes hypotonia, seizures, and cerebral atrophy. Homozygous or compound heterozygous germline pathogenic variants in FH are found in individuals with FHD.[17,18] To date, RCC has not been reported in FHD-affected individuals, possibly because most individuals with FHD survive only a few months with very few surviving to early adulthood.[19] However, a parent (heterozygous carrier) of an individual with FHD developed cutaneous leiomyomas similar to those observed in HLRCC.[2] Four FH variants are thought to be associated with FHD: (1) p.Lys477dup, (2) p.Pro174Arg, (3) p.Gln376Pro, and (4) p.Ala308Gly.[20] The most common variant found in individuals with FHD is the in-frame duplication, c.1431_1433dupAAA (also known as p.Lys477dup). This variant has been observed in 0.5% of the Ashkenazi Jewish population. While multiple studies have demonstrated that certain biallelic FH pathogenic variants can cause autosomal recessive FHD, these variants are not associated with HLRCC when in the heterozygous state.[10,20] Hence, the common FHD variant, p.Lys477dup, is not thought to be associated with an increased risk of RCC. However, the p.Lys477dup variant is associated with autosomal recessive FHD when found in conjunction with another FH variant (i.e., p.Lys477dup on one allele and a different FH variant on the other allele) and not when it is in the homozygous state (i.e., when an individual carries two p.Lys477dup variants). This finding suggests that the p.Lys477dup variant has some residual function. Individuals in these studies who carried the FH p.Lys477dup variant and had RCC shared similarities with individuals who had sporadic forms of kidney cancer, like higher prevalences of clear cell RCC and later ages of RCC onset. SomaticFHvariants Biallelic somatic loss of FH has been identified in two early-onset sporadic uterine leiomyomas and a soft tissue sarcoma of the lower limb without other associated tumor characteristics of the heritable disease.[21,22] Few somatic FH variants have been identified in sporadic forms of RCC.[21,23] References: The mechanisms by which alterations in FH lead to hereditary leiomyomatosis and renal cell cancer (HLRCC) are currently under investigation. Biallelic inactivation of FH has been shown to result in loss of oxidative phosphorylation and reliance on aerobic glycolysis to meet cellular energy requirements. Interruption of the Krebs cycle because of reduced or absent fumarate hydratase activity results in increased levels of intracellular fumarate. This increase inhibits the activity of hypoxia-inducible factor (HIF) prolyl hydroxylases, resulting in the accumulation of HIF-alpha.[1,2] Inactivating variants of FH also appear to result in the generation of reactive oxygen species, further contributing to the stabilization of HIF-alpha.[3] Activation of the HIF pathway leads to a pseudohypoxic state and an upregulation of a transcriptional program contributing to aggressive tumor growth.[4] In addition, accumulated fumarate can activate the antioxidant response pathway which enables cancer cells to survive in an environment of oxidative stress. Fumarate, an electrophile, is able to posttranslationally modify KEAP1 by succination on cysteine sulfhydryls,[5] thereby releasing KEAP1 inhibition of NRF2. The resultant stabilization of NRF2 leads to transcriptional upregulation of antioxidant response element–controlled genes such as AKR1B10, possibly contributing to the neoplastic process.[6] References: The clinical characteristics of hereditary leiomyomatosis and renal cell cancer (HLRCC) include cutaneous leiomyomas, uterine leiomyomas (fibroids), and renal cell cancer (RCC). Affected individuals may have multiple cutaneous leiomyomas, a single skin leiomyoma, or no cutaneous lesion; an RCC that is typically solitary, or no renal tumors; and/or uterine leiomyomas. HLRCC is phenotypically variable; disease severity shows significant intrafamilial and interfamilial variation.[1,2,3] Cutaneous Leiomyomas Cutaneous leiomyomas present as firm papules or nodules that appear pink or reddish-brown. These lesions usually appear on the trunk, on the extremities, and occasionally on the face. These lesions occur at a mean age of 25 years (age range, 10–47 y) and often increase in size and number with age. Lesions are sensitive to light touch and/or cold temperature. They can also be painful. Pain is correlated with severity of cutaneous involvement.[3] The presence of multiple cutaneous leiomyomas is often indicative of HLRCC, and therefore, warrants a genetic workup. One series reported the presence of cutaneous leiomyomas in 22 of 48 patients (46%) with a pathogenic or likely pathogenic variant in FH.[4] The same series demonstrated that 18 of 19 individuals (95%) with multiple leiomyomas had a pathogenic variant in FH.[4] Therefore, the presence of a solitary leiomyoma requires careful analysis of an individual's family history. For more information, see the Clinical diagnosis and Differential diagnosis sections. Uterine Leiomyomas The onset of uterine leiomyomas in women with HLRCC occurs at a younger age than in women in the general population. The age at diagnosis ranges from 18 to 63 years (mean age, 30 y). One series reported uterine leiomyomas in 18 of 29 women (62%) with a pathogenic or likely pathogenic variant in FH; the ages of the women ranged from 24 to 63 years.[4] Uterine leiomyomas are usually large and numerous. Most women with HLRCC experience irregular or heavy menstruation and pelvic pain; thus, they require treatment for leiomyomas at a younger age than women in the general population. Women with HLRCC undergo hysterectomy or myomectomy for symptomatic uterine leiomyomas at a younger age (<30 y) than women in the general population (median age, 45 y).[3,5,6,7] Renal Cell Cancers (RCCs) The symptoms of RCC may include hematuria, lower back pain, and a palpable mass. However, a large number of individuals with RCC are asymptomatic. Furthermore, not all individuals with HLRCC present with or develop RCC. Most RCCs are unilateral and solitary; in a few individuals, they are multifocal. The exact incidence of RCC in affected individuals remains to be determined, and widely varying estimates have been provided by different groups (1%–60%).[1,3,8] The incidence appears to vary on the basis of where the study was performed, the referral patterns of individual groups, and the extent to which individuals were screened for RCC. In studies from the National Cancer Institute (NCI), RCC was identified in approximately 32% of families evaluated.[1,3] The median age at detection of RCC was 37 years,[9] although some cases have been reported to occur as early as age 10 years.[10] Another large series of 135 patients estimated that the lifetime risk was 20.8% by age 85 years.[11] In contrast to other hereditary RCC syndromes, RCCs associated with HLRCC are aggressive,[12,13] with a Fuhrman nuclear grade of 3 or 4 in many cases and 9 of 13 individuals dying from metastatic disease within 5 years of diagnosis.[3]Figure 1 depicts RCCs in a patient with HLRCC. Uterine Leiomyosarcomas It is unclear whether women with HLRCC have a higher risk of developing uterine leiomyosarcomas than women of similar age in the general population. In the original description of HLRCC, it was reported that 2 of 11 women with uterine leiomyomas also had a uterine leiomyosarcoma, a cancer that may be clinically aggressive if not detected and treated at an early stage.[2] To date, germline pathogenic variants in FH have been reported in six women with uterine leiomyosarcoma.[14,15] It seems that most FH pathogenic variant–positive families are not highly predisposed to uterine cancer, but a few individuals and families appear to be at high risk. In North American studies, no uterine leiomyosarcomas in HLRCC individuals or families have been reported.[3] Therefore, the risk of uterine leiomyosarcoma in women with HLRCC is uncertain. This is a question in urgent need of a definitive answer. Other Manifestations Four FH-positive cases with breast cancer, one case of bladder cancer, and one case of bilateral macronodular adrenocortical disease with Cushing syndrome have been reported. A series from the NCI found that 20 of 255 patients (7.8%) with HLRCC had adrenal nodules, some of which did not appear to be adenomas based on imaging characteristics. Resections were performed on many of these lesions since they were fluorodeoxyglucose avid. All of the lesions showed evidence of both micronodular and macronodular adrenal hyperplasia, suggesting that adrenal nodules could be an additional manifestation of HLRCC.[16] It remains to be determined if these manifestations are truly part of the HLRCC phenotype.[6,14,17] Similarly, pheochromocytomas (PHEOS) have been reported in the adrenal glands of individuals with HLRCC.[8,18] However, one of the largest cohorts from the United Kingdom did not report PHEOs in individuals with HLRCC. Therefore, surveillance of PHEOs is not recommended unless further evidence shows that this tumor is part of the HLRCC phenotype.[11] References: Cutaneous Leiomyomas Cutaneous leiomyomas are believed to arise from the arrectores pilorum muscles attached to the hair follicles. Histologically, these are dermal tumors that spare the epidermis. Morphologically, these tumors have interlacing smooth muscle fibers interspersed with collagen fibers.[1] Uterine Leiomyomas A review of the National Cancer Institute's experience with hereditary leiomyomatosis and renal cell cancer (HLRCC)-associated uterine leiomyomas reported that most of these cases were well-circumscribed fascicular tumors with occasional cases showing increased cellularity and atypia. The hallmark feature of these cases was similar to those observed in HLRCC kidney cancer: the presence of orangeophilic, prominent nucleoli that are surrounded by a perinuclear halo. While some cases had atypical features, no cases had tumor necrosis or atypical mitosis suggestive of malignancy or leiomyosarcoma.[2] RCC The renal cell cancers (RCCs) associated with HLRCC have unique histological features, including the presence of cells with abundant amphophilic cytoplasm and large nuclei with large inclusion-like eosinophilic nucleoli. These cytologic features were attributed to type 2 papillary tumors in the original description.[3] However, early studies reported that HLRCC is associated with a spectrum of renal tumors ranging from type 2 papillary to tubulopapillary to collecting duct carcinoma.[4,5] RCC associated with HLRCC may constitute a new renal pathologic entity or a unique HLRCC type. Two studies reported the morphologic spectrum of RCC in HLRCC syndrome after histological examinations of 40 RCCs from 38 patients with germline FHpathogenic variants and HLRCC family histories.[5,6] A number of histological patterns were seen, including cystic, tubulopapillary, tubulo-solid, and often mixed patterns.[5,6] References: Diagnosis and Testing Genetic testing for the FHgene is clinically available and performed by Clinical Laboratory Improvement Amendments (CLIA)-certified laboratories. FH currently is the only gene known to be associated with hereditary leiomyomatosis and renal cell cancer (HLRCC). Most patients with HLRCC have a germline pathogenic variant in FH. Because the genetic analysis of HLRCC is complex, any interpretation of a variant of unknown significance result needs to be performed with consultation by clinical cancer geneticists, ideally in a center that has significant experience with this disease. Clinical diagnosis There is no current consensus on the diagnostic criteria for HLRCC.[1] Available guidelines were created during a previous era of histological classification when FH-deficient papillary renal cell carcinoma (RCC) was classified as type 2 papillary RCC. Suggested guidelines may need to be updated based on this RCC classification change, the availability of immunohistochemical stains to identify loss of FH, and the presence of 2SC in tissue manifestations. Some experts suggest that a clinical dermatologic diagnosis of HLRCC requires one of the following:[2] More recent comprehensive criteria for diagnosis have been suggested and are often used by experts in the field. Suggested criteria include dermatologic manifestations like multiple cutaneous leiomyomas (histologically confirmed). At least two of the following manifestations must also be present:[3,4] Since FH-deficient RCC can resemble collecting duct RCC, the presence of FH-deficient RCC before age 40 years has been suggested as an additional criterion.[5] Patients with seemingly sporadic tumors who have a negative family history and a single, histologically confirmed cutaneous leiomyoma may test positive for the presence of a germline FH pathogenic variant. Although the percentage of germline pathogenic variants in these patient populations is unknown, many centers may refer patients with a single cutaneous leiomyoma for genetic counseling and testing, regardless of family history.[6] Differential diagnosis Cutaneous lesions Cutaneous leiomyomas are rare. The detection of multiple lesions is specific to HLRCC. Because leiomyomas are clinically similar to various cutaneous lesions, histological diagnosis is required to objectively prove the nature of the lesion. Uterine leiomyomas Uterine leiomyoma is the most common benign pelvic tumor in women in the general population. Most uterine leiomyomas are sporadic and nonsyndromic.[7] RCCs Diagnostic clues of HLRCC may rely on the presence of several phenotypic features in different organs (cutaneous, uterine, and renal). One or more of these characteristic features may be present in the patient or in one or more of their affected biologic relatives. Although familial RCCs are associated with rather specific renal pathology, the rarity of these syndromes results in few pathologists gaining sufficient experience to recognize their histological features. The differential diagnoses may include other rare familial RCC syndromes with specific renal pathology, including: Genetic testing Genetic testing is used clinically for diagnostic confirmation of at-risk individuals. It is recommended that both pretest and posttest genetic counseling be offered to persons contemplating germline pathogenic variant testing.[12] Laboratories offering genetic testing for use in clinical decision making must be certified under CLIA laws.[13] Testing strategy Genetic testing for a germline FH pathogenic variant is indicated for all individuals with HLRCC and for all individuals who are suspected of having HLRCC, regardless of family history. This includes individuals with cutaneous leiomyomas, as described in the Clinical diagnosis section of this summary, and individuals who have renal tumors with histological characteristics consistent with HLRCC.[4,14,15] For more information, see the Histopathology section. Risk to family members HLRCC is inherited in an autosomal dominant manner.[16] If a parent of a proband is clinically affected or has a disease-causing variant, the siblings of the proband have a 50% chance of inheriting the pathogenic variant. Each child of an individual with HLRCC has a 50% chance of inheriting the pathogenic variant. The degree of clinical severity is not predictable. Prenatal genetic testing may be available in laboratories offering custom prenatal testing for families in which a pathogenic variant has been identified in an affected family member. Parents of a proband Although some individuals diagnosed with HLRCC have an affected parent, the family history may appear to be negative because of limited family history, failure to recognize the disorder in family members, early death of the affected parent before the onset of syndrome-related symptoms, or late onset of the disease in the affected parent.[17] Siblings of a proband Testing of at-risk family members Use of genetic testing for early identification of at-risk family members improves diagnostic certainty. It reduces the number of unnecessary costly and stressful screening procedures in at-risk members who have not inherited their family's disease-causing variant.[13,18,19] Early recognition of clinical manifestations may allow timely intervention, which could, in theory, improve outcome. Therefore, clinical surveillance of asymptomatic at-risk relatives for early RCC detection is reasonable, but additional objective data regarding the impact of screening on syndrome-related mortality are needed. Related genetic counseling issues Predicting the phenotype in individuals who have inherited a pathogenic variant It is not possible to predict whether HLRCC-related symptoms will occur or, if they do, what the age at onset, type, severity, or clinical characteristics will be in individuals who have a pathogenic variant. In an in-depth characterization of clinical and genetic features analyzed within 21 new families, the phenotypes displayed a wide range of clinical presentations and no apparent genotype -phenotype correlations were found.[20] When neither parent of a proband with an autosomal dominant condition has the disease-causing variant or clinical evidence of the disorder, it is likely that the proband has a de novo pathogenic variant. However, nonmedical explanations include the possibility of alternate paternity or undisclosed adoption. Genetic testing of at-risk family members is appropriate in order to identify the need for continued lifelong clinical surveillance. Interpretation of the pathogenic variant test result is most accurate when a disease-causing variant has been identified in an affected family member. Those who have a disease-causing variant are recommended to undergo lifelong periodic surveillance. Meanwhile, family members and offspring who have not inherited the pathogenic variant are thought to have RCC risks similar to those in the general population; no special management of these individuals is recommended. Early detection of at-risk individuals affects medical management Screening for early disease manifestations in HLRCC is an important aspect of clinical care of affected individuals. Although there are no prospective studies comparing specific renal cancer screening practices, the aggressive nature of HLRCC-associated RCC [3] justifies efforts directed at the early identification of cancer. When tumors are small and localized, partial nephrectomy may be a feasible option; however, the infiltrative nature of these tumors has led some groups to suggest a wide margin must be taken to achieve complete resection.[21] Uterine fibroids often cause significant symptoms related to bleeding and the presence of a large mass, but small fibroids may be asymptomatic. As HLRCC fibroids can lead to hysterectomies and loss of the ability to bear children in affected young women, the goal of screening in women interested in preserving fertility is to limit some of these irreversible complications. Although there are no specific management recommendations related to HLRCC-associated fibroids, various management strategies have proven effective in the treatment of sporadic fibroids. These strategies include use of hormonal therapies, pain medications, percutaneous and endovascular procedures, and surgical options. Early referral to a fertility specialist may be useful to assist with family planning. Surveillance It has been suggested that individuals with a suspected or confirmed diagnosis of HLRCC, individuals with heterozygous pathogenic variants in FH regardless of clinical manifestations, and at-risk family members who have not undergone genetic testing undertake the following regular surveillance, performed by physicians familiar with the clinical manifestations of HLRCC. Any suspicious renal lesion (indeterminate, questionable, or complex cysts) at a previous examination should be closely followed with periodic imaging, preferably using the same modality to allow for comparisons. The use of renal ultrasound examination may be helpful in the characterization of cystic lesions identified on cross-sectional imaging. It should be cautioned that ultrasound examination alone is never sufficient. Renal tumors should be evaluated by a clinician familiar with HLRCC-related renal cancer.[10,24] Because of the aggressive growth of these tumors, patients warrant regular surveillance with a low threshold for early surgical intervention for solid renal lesions. This strategy differs from that described for several other hereditary RCC syndromes, in which the tumor behavior is more indolent, and for which observation may be a viable option.[10,24,25] Level of evidence (skin surveillance): 5 Level of evidence (uterine surveillance): 4 Level of evidence (renal surveillance): 4 Treatment of Manifestations Cutaneous lesions Cutaneous leiomyomas are most appropriately examined by a dermatologist. Generally, asymptomatic cutaneous leiomyomas require no treatment. Treatment of symptomatic cutaneous leiomyomas may be difficult if a patient has diffuse disease in a wide distribution. Surgical excision may be performed for a solitary painful lesion. Lesions can be treated by cryoablation and/or lasers. Several medications, including calcium channel blockers, alpha blockers, nitroglycerin, antidepressants, and antiepileptic drugs, reportedly reduce leiomyoma-related pain.[26] A small, randomized clinical trial (09-C-0072 [NCT00971620]) showed that intralesional injection of botulinum toxin A (Botox) may improve quality of life.[27] Level of evidence: 5 Uterine leiomyomas Uterine leiomyomas are best evaluated by a gynecologist. HLRCC-associated leiomyomas are treated in the same manner as sporadic leiomyomas. However, because of the multiplicity, size, and potential rapid growth observed in HLRCC-related uterine leiomyomas, most women may require medical and/or surgical intervention earlier and more often than would be expected in the general population. Medical therapy (currently including gonadotropin-releasing hormone agonists, anti-hormonal medications, and pain relievers) may be used to initially treat uterine leiomyomas, both to decrease their size in preparation for surgical removal and to provide temporary relief from leiomyoma-related pain. When women desire fertility preservation, myomectomy can be used to remove leiomyomas and simultaneously preserve the uterus. Hysterectomy should be performed only when necessary.[6,7] Level of evidence: 4 RCCs Efforts aimed at early detection of HLRCC-related RCC are prudent, given its biological aggressiveness. However, studies do not currently show that early detection is clearly associated with improved survival. Surgical excision of these malignancies at the first sign of disease is recommended, unlike management of other hereditary cancer syndromes. The propensity for lymph node involvement, even with small renal tumors, may necessitate a lymph node dissection for more appropriate staging.[21] Radical nephrectomy or partial nephrectomy with wide margins should be considered in individuals with detectable renal masses, including small, subcentimetric tumors.[10,24,25] Level of evidence: 4 Therapies under investigation It has been suggested that hypoxia-inducible factor (HIF1)-alpha overexpression is involved in HLRCC tumorigenesis.[28,29] Therefore, potential targeted therapies for HLRCC-associated tumors may include HIF1-alpha targeting agents, when such agents become clinically available. Loss of oxidative phosphorylation resulting from biallelic inactivation of FH renders HLRCC tumors almost entirely reliant on aerobic glycolysis for meeting cellular adenosine triphosphate and other bioenergetics requirements. Consequently, targeting aerobic glycolysis is being explored as a therapeutic strategy.[30,31] A phase II study (10-C-0114 [NCT01130519]) examining the combination of bevacizumab and erlotinib for the treatment of advanced HLRCC is ongoing and is based partly on the premise that this combination might inhibit effective glucose delivery to tumor cells.[32] Other investigations [33] evaluating the known consequences of FH inactivation in HLRCC kidney cancer have confirmed that there are very high levels of NAD(P)H dehydrogenase quinine 1 (NQO1) expression in HLRCC kidney tumors. Expression of this compound is lower in other types of hereditary RCC, including the clear cell RCC associated with von Hippel-Lindau disease and the papillary RCC associated with HPRC. The activation of an oxidative stress response pathway mediated by NRF2, a transcription factor that regulates the transcription of NQO1, could explain NQO1 overexpression in these tumors. Vandetanib, an oral VEGFR2 and EGFR inhibitor with additional activity against Abl-1 kinase, has potent activity against FH-deficient cells in vitro and induces regression of HLRCC-derived xenografts in mice. The activity of vandetanib in this model is mediated, at least in part, by its ability to disrupt the NRF2-mediated cytoprotective oxidative stress response pathway in an Abl-dependent fashion. Furthermore, metformin, an activator of 5'–AMP activated protein kinase (AMPK), was synergistic with vandetanib both in vitro and in mouse xenografts derived from FH-deficient human renal cancer.[34] These data provided the basis for a clinical trial (NCT02495103) to evaluate the efficacy of this combination in HLRCC patients with advanced kidney cancer. General information about clinical trials is also available from the NCI website. References: Prognosis is quite good for cutaneous and uterine manifestations of hereditary leiomyomatosis and renal cell cancer (HLRCC). Local management of cutaneous manifestations, when required, and hysterectomy, where indicated, address these sites fairly effectively and with minimal long-term consequences. The incidence of uterine leiomyosarcomas is likely quite low and is unlikely to substantively affect median survival at a cohort level. Renal cell cancer (RCC) in the context of HLRCC is a considerably more ominous manifestation, and the HLRCC patients who develop RCC [1,2,3,4,5] are at high risk of developing metastatic disease.[6] Metastatic RCC associated with HLRCC is characterized by an aggressive clinical course. There are no sufficiently large patient cohorts or databases that provide a precise estimate of survival in this population; however, retrospective cohorts demonstrate that these cancers have worse outcomes than other conventional forms of RCC.[7] References: There are two major unmet needs, other than the availability of effective medical therapy for metastatic disease, in the management of patients with hereditary leiomyomatosis and renal cell cancer (HLRCC). The first is the ability to predict who will develop renal cell cancer to allow detection earlier and with a higher degree of precision. The development of diagnostic blood-based tests or imaging tools that permit cost-effective surveillance of the kidneys of patients with HLRCC would have a major positive effect on the outcomes of these individuals. The second major unmet need is for a more accurate determination of the genotype -phenotype correlations for various genetic lesions found in the FHgene. New polymorphisms in the FH gene are frequently of uncertain significance, and considerable effort needs to be expended to determine their clinical significance. Devising in silico prediction tools and linking these to robust patient databases and registries will expand our understanding of specific FH gene variants. The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above. Added text to state that available guidelines were created during a previous era of histological classification when FH-deficient papillary renal cell carcinoma (RCC) was classified as type 2 papillary RCC. Suggested guidelines may need to be updated based on this RCC classification change, the availability of immunohistochemical stains to identify loss of FH, and the presence of 2SC in tissue manifestations. Added text about suggested criteria for a hereditary leiomyomatosis and renal cell cancer (HLRCC) diagnosis. Revised text to state that since FH-deficient renal cancer can resemble collecting duct RCC, the presence of FH-deficient RCC before age 40 years has been suggested as an additional criterion for HLRCC diagnosis. This summary is written and maintained by the PDQ Cancer Genetics Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® Cancer Information for Health Professionals pages. Purpose of This Summary This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the genetics of hereditary leiomyomatosis and renal cell cancer. It is intended as a resource to inform and assist clinicians in the care of their patients. It does not provide formal guidelines or recommendations for making health care decisions. Reviewers and Updates This summary is reviewed regularly and updated as necessary by the PDQ Cancer Genetics Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH). Board members review recently published articles each month to determine whether an article should: Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary. The lead reviewers for Hereditary Leiomyomatosis and Renal Cell Cancer are: Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website's Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries. Levels of Evidence Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Cancer Genetics Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations. Permission to Use This Summary PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary]." The preferred citation for this PDQ summary is: PDQ® Cancer Genetics Editorial Board. PDQ Hereditary Leiomyomatosis and Renal Cell Cancer. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/publications/pdq/information-summaries/genetics/hlrcc-syndrome-hp-pdq. Accessed <MM/DD/YYYY>. [PMID: 33724749] Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images. Disclaimer The information in these summaries should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page. Contact Us More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's Email Us. Last Revised: 2024-11-06 This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Ignite Healthwise, LLC.Hereditary Leiomyomatosis and Renal Cell Cancer (PDQ®): Genetics - Health Professional Information [NCI]
Introduction
Genetics
Molecular Biology
Clinical Manifestations
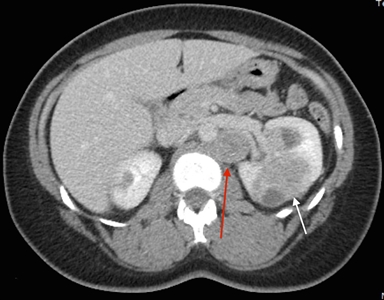
Figure 1. Hereditary leiomyomatosis and renal cell cancer–associated renal tumors are commonly unilateral and solitary; in a few individuals, they are multifocal. Red arrow indicates a retroperitoneal lymph node. White arrow indicates a left renal mass.Histopathology
Management
Prognosis
Future Directions
Latest Updates to This Summary (11 / 06 / 2024)
About This PDQ Summary
Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.Hereditary Leiomyomatosis and Renal Cell Cancer (PDQ®): Genetics - Health Professional Information [NCI]



